Breaking the Cycle of Mental Health Stigma - Psychosocial Support for Refugees in Thailand
Interview with Chitlada Kankeow, Malteser International’s psychosocial support supervisor in camps for displaced persons from Myanmar
When 48-year-old Chitlada Kankeow welcomes me to her workplace, the "Psychosocial Support Unit", that Malteser International runs in two camps in Thailand, I immediately feel at ease - in her calm and friendly presence and in the bright room that, like the other buildings of the Malteser International hospital and all the houses in the camps, is made of bamboo and wood.

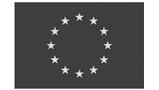
We are at Camp Mae Ra Ma Luang, one of nine so-called "temporary shelters" in northwestern Thailand, just a few kilometers from the border with Myanmar, surrounded by lush green forests that stretch up the surrounding mountains. Around 100,000 people - most of them members of the Karen ethnic group - have found a safe place here in these shelters after they, their parents or grandparents fled violence and persecution in Myanmar. The camps have existed for more than 30 years. Many of the displaced people were born here, have never been to Myanmar. Although it is peaceful and safe here, the prospects and opportunities in the camps are limited. Since they are not legally recognized as refugees, they are not allowed to leave the camps, work, or move freely in their host country. How does such a living situation and the experience of displacement affect people and their mental health? And how can these people be accompanied and supported, even if or precisely because the hopeless conditions and circumstances are not going to change anytime soon?
Chitlada Kankeow and her psychosocial support team are addressing those very questions and are available with various psychosocial services for people in the camps. I sit down with her, and we talk about the importance and challenges of psychosocial support.
What is your job in the camps in Thailand?
Chitlada Kankeow: Actually, I am not a psychiatrist. I am not a psychologist. But I have been a trained psychosocial counselor for many, many years. For Malteser International, I have been working as a psychosocial support supervisor since 2018, almost five years now. One of my main tasks is to train our staff in the camps, especially of course the psychosocial support counselors. There are five in Mae La Oon and five in Mae Ra Ma Luang camp. They belong to the camp-based staff, which means they are refugees themselves. I equip them with the necessary training so that they can provide psychosocial support. I also supervise them in individual and group counseling, as well as in all other activity or services related to psychosocial support. Moreover, I conduct the counseling sessions and other activities with the patients myself. Another part of my job is to facilitate and collaborate with the community-based organizations (organizations in the camps or nearby communities which are usually run by refugees and/or Karen) and the section committees (refugee-led camp management bodies) to conduct community education and to raise awareness on mental health among the camp population.
What is your motivation for this job?

My family is a big family, and my grandfather was a pastor. When I was young, I saw my grandfather helping other people, for example, visiting church members who were not well. And he always told us children that we should help other people when we have the opportunity. When I grew up, his words were still in my heart and mind. Therefore, I am happy that in my profession I can help people and support them to feel good again.Other words that motivate me and that I like are from a speech by Barack Obama. He said, “If you go out and make some good things happen, you will fill the world with hope”. In my opinion, it shows that doing good things doesn’t have to be the big action, the big commitment. Seemingly small things, like listening to others and letting them express themselves, make people feel better.
Why is psychosocial support so important - in general and in the context of displacement?
Psychosocial support is absolutely very important, and with all the changes in the world, it’s becoming more and more important. These are things that affect everyone: Globalization, social media, changing relationships, diseases and pandemics like COVID-19 that are on the rise. If you haven’t learned how to cope emotionally in such a world, and you feel insecure, then your mental health suffers. That’s why I think psychosocial support is very important for everyone. In the refugee camps, a lot of people don't know if their situation will change in the future. They don’t know what will happen. They ask themselves: do I have to or should I return to Myanmar, even if it is still not safe? Others dream of going to a third country, but the opportunities are rare and it is hardly an option, a lot of countries are closed to them. So they don’t know what their future will be, thus they suffer and are depressed.
How do people in the camps find you? How do they learn about your services?

Some patients come to us or are referred to us after they receive medical services in our inpatient or outpatient departments. Others are sent to us by our Community Health Workers who do outreach in the camp community. Some patients we receive from other organizations working in the camps that may also refer patients to us. My team also visits households in the camps. This makes it easier for some people to come and meet us because they already know us. Others come because they heard about our service from one of our patients. So they come by themselves to talk to us. We've found that it's very helpful to go into the outpatient and inpatient departments to just greet patients and talk to them and let them know that our mental health support services are available and that we care about them. I think that's very important.
What does psychosocial support look like in the refugee camps in Thailand?
We offer individual and group counseling. A patient who receives individual counseling also participates in group counseling. Here, our patients have the opportunity to share their experiences, but are also encouraged to counsel their friends in the group. In this way, they can learn from each other, see how other people deal with mental health issues, and experience that they are not alone in this. In addition to counseling, we also offer relaxation activities such as breathing exercises, massages, and yoga. Especially our teenagers are happy to do yoga. These physical exercises are important because mental health problems are often accompanied by physical complaints, for example, fatigue or breathing problems. These relaxation exercises really help them, they feel better afterwards. We also have them practice at their homes. When they come back, we ask how they feel with these practices. But it’s not for everyone. If it doesn’t work for a person, we have other tools for them. We also visit our patients and other community members at home and do outreach in the camps. In the end, it's not just our job as a psychosocial support team to take care of people's mental health. All the MI staff working in the camps, whether they're medics, doctors or nutritionists, they do it as well – in small ways. We look at our patients holistically, and even a short question like “How are you feeling?” can make someone feel better or make all the difference.
How is psychosocial support received by the camp population? Are there stigmas or reluctances?
I think the stigma associated with mental health problems is similar all over the world. In Karen culture, it's common not to express yourself emotionally and not to talk about what's going on inside you. Yes, we have struggled with the stigma in the past. For example, some people said our place was for psychopaths. But fortunately there is a solution: education. We explain to the community what we do and why it's important. Also, patients who come to us tell people close to them that they feel better after talking to us, which also supports our message. Educating and promoting understanding - this helps break the cycle of stigma so that people change their minds about mental health services from "this is for psychopaths" to "this helps people feel better." On an individual level, building a relationship with patients is critical so they learn and know they can trust us. The first thing we do is let them talk and express themselves. That's how we start, and over time they open up more and more.
Why do people come to you? What mental health issues do people struggle with here?
Almost all people who come to our psychosocial support team initially complain of physical problems. After talking and spending time together, most people realize that it's not a physical problem, but that it has to do with their mental health. The majority of patients suffer from depression, which is usually a consequence of the trauma they experienced before and during their displacement from Myanmar. The symptoms I see on a regular basis are that the patients are really suffering and can't cope anymore. Usually, they have a whole range of symptoms before they finally come to us. We then check with them to see how their mental health issues are manifesting, with questions like: Do you feel lethargic and don't want to talk to anyone? Do you have trouble sleeping at night? Do you feel anxious for no reason? And so on. This way we can find out what specific problem the patient is dealing with. Since I am not a psychologist or psychiatrist, I must add that we cannot treat and help everyone on our own, as mental health is a very sensitive issue. That is why we work closely with other professionals. A psychiatrist from Thailand advises us on the more severe cases. Sometimes this also means that we have to refer a patient to a Thai hospital outside the camp.
You have been working in the camps for over four years. Have you noticed a change regarding mental health?

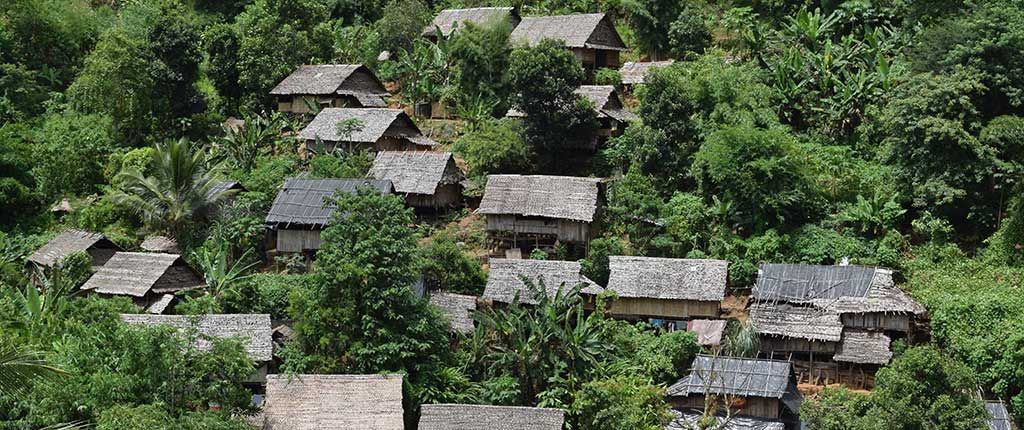
We have more patients now than we used to, but that doesn't mean there are more mental health problems among the refugees than there were a few years ago. It mainly shows that they know about our service and more and more people are not afraid to use it. This is actually a good sign, because it shows that more people are aware of mental health and its importance. This is also a result of our awareness-raising activities that we carry out together with the Section Committee. In this regard, it is very important to us that the refugee community takes responsibility. For example, on World Mental Health Day, we involve the community in all planning and activities.
How do you take care of yourself?
We help people, so we have to look after ourselves as well. We provide counseling to each other in our team; it's like group care. We invite our employees to sit down and talk about any challenge, any problem, and encourage them to share their experiences. I also give the psychosocial support staff tips on how to relieve stress, such as massage, breathing exercises, etc. I personally like the breathing exercises and positive thinking. Every day I think about: What makes me happy today? What are my little moments of happiness? We also offer this exercise for our patients.
What touches you in your daily work?
I really love working in this context and with the refugees. My staff shared with me that a patient recently told them that just meeting and talking to us makes the person feel better. Hearing something like this makes me proud.
This interview was conducted by Anne Hensel in September 2022.
Our work in Thailand
Since 1993, Malteser International has been implementing a wide-ranging primary health care project for currently about 18,000 refugees in the two refugee camps Mae Ra Ma Luang and Mae La Oon on the Thai-Myanmar border. Our project includes both comprehensive curative and preventative measures to improve the health status of the refugees, as well as the provision of water, sanitation, and hygiene. In addition to medical treatment in our hospital wards, we take care of, among other things, the referral of severe cases to Thai hospitals, prevention and control of communicable disease outbreaks such as COVID-19, we accompany mothers and their babies during and after pregnancy and delivery, provide therapeutic and complementary foods for malnourished children, and offer psychosocial support. This is possible thanks to the financial support through the European Union, other donors and private donations.